The Covid-19 pandemic is unlike anything the world has seen for generations and as a result, few, if any countries were set up for the immediacy and scale of the impact. A pandemic of this size has put pressure on all of our services. With social distancing measures being gradually eased - albeit with baited breath and localised strategies - now, the combination of testing and digital solutions are important in helping to contain the current pandemic and avoid a second peak in the coming weeks and months.
Many health-tech providers are working with the NHS for example, Microsoft Teams has been rolled out across the entire NHS to support remote working. Matt Hancock has urged the NHS to shift towards "Zoom medicine", where patients can engage with doctors via the phone or using video conferencing tools to reduce face-to face appointments.
It appears that the doubts and questions that people in the health sector have had around the use of technology have taken a back seat. Why? Because the industry is looking for ways to deliver effective and scalable healthcare, whilst keeping people away from hospitals, surgeries and clinics where possible. With a lot of innovation being fast-tracked into mainstream healthcare delivery, it will be impossible to put these solutions back post-pandemic. Before our eyes technology is shaping how healthcare will be delivered in the years to come.
Adjusting to the new normal
An outbreak such as this is daunting for anyone, but for people living with cancer, they have had to contend with the added concerns and challenges of changes or postponements to their treatment. At the beginning of the pandemic, new patients were forced to delay starting their treatment until after the worst of the outbreak had passed. We also saw news of people with less than a year to live, being put at the back of the NHS queue. The action taken to scale back urgent treatment and the public’s apprehension of going for referral assessments has caused concerns that a post-Covid cancer surge is heading our way. Recent research has suggested that almost 35,000 more people with cancer in England could die within a year as a result of the pandemic.
Although NHS services are being restored, starting with cancer and mental health, doctors are now faced with a series of new challenges, including how to prioritise who is treated first. Charities such as Pancreatic Cancer UK are petitioning the NHS and the government with its 'No Time To Wait' campaign to address this emergency and avoid certain patients being pushed to the back of the queue.
Currently a framework of questions and visual observations are used by clinical teams to determine the health-status of patients. This is where a data-driven approach can play a dramatic role in helping to better inform doctors and nurses. It will also help take the guesswork out of treatment for patients.
The connected patient
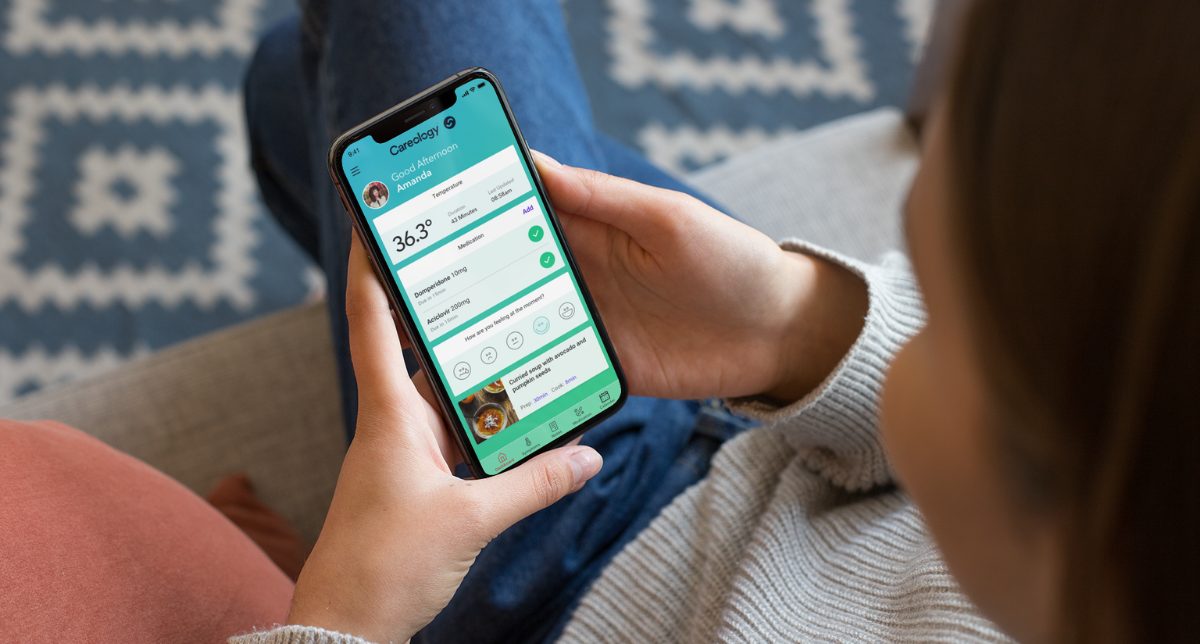
Cancer is a hugely complex disease and it is hard to expect patients to become experts and recall every detail of what they have experienced over a period of time. A common side-effect for people undergoing chemotherapy treatment is short-term memory loss, often described as “chemo brain”. Having a digital tool where they can monitor their symptoms, medications, side-effects and more using connected wearable technologies, provides a more accurate and trusted view. It also means health professionals will be able to access a 360º view of the patient whether they are seeing them in person or remotely via video consultation. This will help doctors to deliver better patient care and save more lives.
In an increasingly isolated world, it's about making sure that people living and dealing with cancer feel supported. By utilising the data available to them, clinicians can identify side-effects and symptoms quickly, and spot at a glance whether somebody under their care needs to come in for further treatment, or needs advice whilst at home. This will help lighten the load on hospitals, and increase capacity as they can take a data-led approach to triage.
A key area which has prompted a lot of discussion during lock down is around mental health. Staying at home for extended periods of time can be difficult. But for people living with an illness, anxiety and loneliness can slowly creep in and wreak havoc with an individual's mental state. Being able to track mood and mental state online which clinical professionals have visibility of will be key to make sure prompt action is taking place to avoid symptoms of depression. Regularly logging thoughts can unburden people and make them feel less lonely, especially at a time of self-isolation. With some regions across the UK going back into lockdown as cases begin to creep up, staying connected will remain a key part of patient treatment.
Wearable technology devices can be used to monitor physicality changes. This way, vulnerable members of society will no longer need to have an internal tug of war and debate on whether they should report side-effects and symptoms to their clinicians.
We are on the cusp of a healthtech revolution where the lessons learned from this virus and approach to tackling it today will become embedded for years to come offering more safe, scalable and efficient healthcare.
This article was first published in Healthcare Global.